DISCLAIMER
The draft recommendations contained herein were preliminary drafts submitted for discussion purposes only and do not constitute final determinations. They have been subject to modification, substitution, or rejection and may not reflect the adopted positions of IFATCA. For the most current version of all official policies, including the identification of any documents that have been superseded or amended, please refer to the IFATCA Technical and Professional Manual (TPM).
53RD ANNUAL CONFERENCE, Gran Canaria, Spain, 5-9 May 2014WP No. 161Sleep Apnea and ObesityPresented by PLC |
Summary
This paper considers the relationship between Obstructive Sleep Apnea (OSA) and Obesity, regarding FAA’s intentions for new policy checking overweight pilots and ATCOs for OSA.
Introduction
1.1 At Conference in Dubrovnik in 2009, PLC presented an information paper dealing with sleep apnea, as part of fatigue management in aviation. Recently, after several highly publicised incidents involving sleeping or fatigued pilots and air traffic controllers, the U.S Federal Aviation Administration (FAA) introduced new policy intentions, requiring all overweight pilots and controllers to undergo testing for sleep disorders. Regarding that, PLC thought this issue should be investigated and be brought to the attention of all MAs.
Discussion
2.1 Sleep apnea
Sleep apnea is one of a variety of sleep disorders. Literature on the subject refers to the most common type of sleep apnea called Obstructive Sleep Apnea (OSA), which is defined as a sleep disorder characterised by intermittent complete or partial upper airway collapse during sleep, resulting in frequent episodes of apnea. The ensuring reduction of airflow often leads to acute derangements in gas exchange and recurrent arousals from sleep. Symptoms such as habitual, loud snoring, nocturnal breathing pauses, choking and gasping are well identified with OSA, which is recognised as an important cause of medical morbidity and mortality. The health consequences of OSA are numerous. Individuals with the disorder often complain of morning headaches, constant fatigue, listlessness and moodiness. If left untreated, OSA leads to excessive daytime sleepiness, fatigue, cognitive dysfunction, impaired work performance and decrements in health- related quality of life. It also increases the risk of high blood pressure, high heart rate, stroke and obesity.
2.1.1 Risk Factors
Literature describes a correlation between many factors and OSA. Demographic aspects reflect that OSA is more common among males aged 40-70 with familial background. The prevalence of OSA is 2–3% and 4–5% in middle-aged women and men, respectively.
Genetics, smoking, menopause, alcohol use before sleep and night time nasal congestion are all suspected to increase the probability of OSA.
In addition, established risk factors for OSA are being overweight and obesity, central body fat distribution, large neck girth and craniofacial and upper airway abnormalities.
The prevalence of OSA among obese patients exceeds 30%, and 60-90% of adults with OSA are overweight. These facts are likely indicators that obesity is probably one of the most important risk factors for the development of OSA.
Because OSA is linked to several risk factors and associated diseases, several epidemiological studies reported on increased prevalence of OSA in patients with hypothyroidism, diabetes, gastro- esophageal reflux, and others. In populations with cardiovascular diseases, the prevalence has been found to be substantially increased, especially in patients with hypertension. The prevalence has been also reported to be increased in patients with stroke, renal failure, and heart failure.
2.2 Essential sleep science
ICAO Doc. 9966 (FRMS manual for regulators) looks at sleep science, and emphasises that there are a variety of ways of looking at what is happening in the sleeping brain. Also, there are three important parameters being studied in sleep research: brain waves, eye movements and muscle tone.
An important term used with respect to sleep is the circadian body clock, which is a neural pacemaker in the brain that monitors the day/night cycle (via a special light input pathway from the eyes) and determines our preference for sleeping at night. Shift work is problematic because it requires a shift in the sleep/wake pattern that is resisted by the circadian body clock, which remains “locked on” to the day/night cycle. Almost every aspect of human functioning (physical or mental) undergoes daily cycles that are influenced by the circadian body clock.
2.2.1 It is possible to identify two very different kinds of sleep:
a. Non-rapid eye movement sleep (Non REM sleep) – involves gradual slowing of the brainwaves, heart rate and breathing tend to be slow and regular. People woken from non-REM sleep do not usually recall much mental activity.
Non-REM sleep is usually divided into four stages, based on the characteristics of the brainwaves. Stages 1 and 2 represent lighter sleep, and stages 3 and 4 represent deeper sleep and are often described as slow-wave sleep.
Slow-wave sleep has a number of important properties: the longer you are awake, the more slow-wave sleep you will have in your next sleep period and across a sleep period, the proportion of time spent in slow-wave sleep decreases. In slow-wave sleep, the brain is still about 80 per cent activated and capable of active cognitive processing. There is growing evidence that slowwave sleep is essential for the consolidation of some types of memory and is therefore necessary for learning.
b. Rapid eye movement sleep (REM sleep) – brain activity looks similar to brain activity during waking. People woken from REM sleep can typically recall vivid dreaming. At the same time, the body cannot move in response to signals from the brain so dreams cannot be acted out. People vary greatly in their ability to recall dreams, and we generally only recall them when we wake spontaneously out of REM sleep. Nevertheless, most adults normally spend about a quarter of their sleep time in REM sleep.
Across a normal night of sleep, non-REM sleep and REM sleep alternate in a cycle that lasts roughly 90 minutes. The amount of slow-wave sleep in each non-REM/ REM cycle decreases across the night, and there may be none at all in the later cycles. In contrast, the amount of REM sleep in each non-REM/ REM cycle increases across the night. Interestingly, slow-wave sleep always predominates at the beginning of a sleep period, regardless of when sleep occurs in the day/ night cycle or in the circadian body clock cycle. In contrast, the time from sleep onset to the first bout of REM (the REM latency) and the duration of each REM bout varies markedly across the circadian body clock cycle. The circadian drive for REM sleep is strongest a few hours before normal wakeup time.
When someone is suffering from sleep loss, restoration of a normal non-REM/ REM cycle is one measure of recovery from the effects of it. Lost sleep is not recovered hour-for-hour, although recovery sleep may be slightly longer than usual.
2.2.2 Sleep quality
Sleep quality depends on going through unbroken non-REM/ REM cycles (which suggests that both types of sleep are necessary and one is not more important than the other). The more the non-REM/ REM cycle is fragmented by waking up, or by arousals that move the brain to a lighter stage of sleep without actually waking up, the less restorative value sleep has in terms of how you feel and function the next day.
In aviation world, because uninterrupted non-REM/ REM cycles are the key to good quality sleep, operators should develop procedures that minimise interruptions to crew members’ and ATCOs’ sleep. Operators should also develop procedures to protect sleep at layover and napping facilities.
The quality of sleep can also be disrupted by a wide variety of sleep disorders, which make it impossible to obtain restorative sleep, even when people spend enough time trying to sleep.
2.2.3 Amount of sleep
- Sleep restriction is common in flight operations.
- Not getting enough sleep leads to: feeling sleepier, difficulty staying alert, getting irritable, slower reactions, poorer coordination, slower thinking, getting fixated on part of a problem and losing the big picture (loss of situation awareness), less creative problem solving, and reduced memory consolidation (impaired learning).
- Lost hours of sleep do not need to be recovered hour-for-hour.
- At least two consecutive nights of unrestricted sleep are required to recover from the cumulative effects of multiple nights of restricted sleep.
- Controlled napping can temporarily relieve the symptoms of sleep loss.
2.2.4 Shift work
From the perspective of human physiology, shift work can be defined as any duty pattern that requires a crew member to be awake during the time in the circadian body clock cycle that they would normally be asleep. Night duty is a part of shift work for crew members and ATCOs, and forces them to sleep later than normal in their circadian body clock cycle. This means that they have a limited amount of time to sleep before the circadian body clock wakes them up.
Discoveries in sleep science and circadian rhythms provide a strong scientific basis for FRMS. The science does not address every detailed operational question, and since new evidence and professional experience are accrued, it never will. In other words, there will always be a need to combine operational experience and scientific knowledge to come up with workable controls and mitigations to manage fatigue risk.
2.3 Overweight and Obesity
Overweight and obesity are defined as abnormal or excessive fat accumulation that may impair health. A simple index that is commonly used to classify overweight and obesity in adults is the Body Mass Index (BMI). It is a simple index of weight-forheight and defined as a person’s weight in kilograms divided by the square of his height in meters (kg/m2).
The World Health Organisation (WHO) defines:
- Overweight- a BMI greater than or equal to 25.
- Obesity- a BMI greater or equal to 30.
BMI greater than 40 is commonly defined as Morbid Obesity. Overweight and obesity are the fifth leading risk for global deaths. At least 2.8 million adults die each year as a result of being overweight or obese. What causes people to be overweight and obesity is an energy imbalance between calories consumed and calories expended. Globally, there has been an increased intake of energy-dense foods that are high in fat, and an increase in physical inactivity due to the increasingly sedentary nature of many forms of work, changing modes of transportation, and increasing urbanisation.
2.4 FAA’s new policy intentions
The FAA proposed a new policy, whereby all pilots and controllers will be screened during their routine medical examinations. Those with a body mass index (BMI) of 40 or greater and a neck circumference of 17 inches would have to be tested for OSA. At the time of presenting this WP, the new policy is suspended.
ALPA approach to FAA’s new policy intentions
The Air Line Pilots Association (ALPA) issued a statement in support of legislation that passed the U.S House of Representatives on February 11th 2014, which requires the FAA to follow the appropriate rulemaking process in order to make any changes to medical certification for pilots and ATCOs regarding sleep apnea:
“ALPA applauds the U.S House Representatives for passing bipartisan legislation that ensures that any FAA policy changes to a pilot’s medical certificate related to OSA will go through a proper rulemaking process that includes input from industry stakeholders. The FAA had proposed to require that aviation medical examiners calculate the BMI for each pilot and ATCO, requiring that applicants with a BMI of 40 or more be evaluated by a physician who is a board- certified sleep specialist. ALPA believes that this single- criteria approach should be replaced by one which takes into account the pilot’s medical history, and one which provides ample time for a pilot who suffers from OSA to address it before putting his or her medical certificate at risk.”
(Air Transport news – 12th Feb 2014)
2.5 OSA and Obesity – The Chicken or the Egg?
Excess body weight is one of the risk factors for sleep disorders. As mentioned, OSA is much more common in obese individuals. It is believed that the airway of the obese individual becomes obstructed by large tonsils, enlarged tongue and increased fat in the neck, all pressing on the airway when the throat muscles are relaxed with sleep.
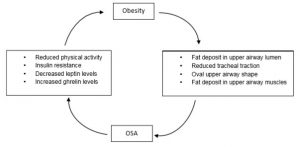
There are several mechanisms responsible for the increased risk of OSA with obesity. These include reduced pharyngeal lumen size due to fatty tissue within the airway or in its lateral walls, decreased upper airway muscle protective force due to fatty deposits in the muscle, and reduced upper airway size secondary to mass effect of the large abdomen on the chest wall and tracheal traction.
While it is well documented that obesity can result in OSA via several mechanisms, recent evidence suggests that OSA can worsen obesity. Thus, it appears that there are complex associations between OSA and obesity.
Many studies on sleep discuss the relevant issue of quality versus quantity. It is already well known that among people working on shifts, such as ATCOs, the quality of sleep is often more important than its quantity. As discussed in PLC’s previous paper on OSA (2009), OSA influences sleep quality and can lead to daytime sleepiness. Daytime sleepiness may result in decreased mood and decreased physical activity, which if not associated with reduced caloric intake, will obviously worsen obesity. Indeed, it has been shown that obesity and OSA are associated with reduced physical activity. When suffering from apneas during sleep, which leads to daytime sleepiness, it may be much harder to begin an exercise program or to sustain one. Thus, theoretically patients with OSA are at high risk of gaining weight and subsequently worsening their OSA. When treated, patients manage to improve alertness and daytime activity. If remained untreated, some patients tend to gain weight and the apnea becomes worse.
2.5.1 Hormonal influence
The metabolic balance of sleep apnea and obesity seems to result from a complex balance between several regulatory hormones. First hormone to be associated with lack of sleep is insulin, which has the main role in glucose metabolism and balancing blood glucose levels. Epidemiological evidence supports an association between chronic partial sleep deprivation (short sleep duration) and the risk for obesity, insulin resistance, and diabetes. Furthermore, sleep deprivation decreases glucose tolerance and results insulin resistance, which is a physiological condition in which cells fail to respond to the normal actions of insulin and cause high blood glucose levels. Since OSA is associated with sleep fragmentation, effectively sleep loss and daytime sleepiness, the insulin sensitivity in patients with OSA has been assessed and indeed insulin resistance has been reported.
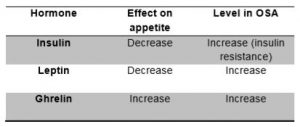
Two other hormones believed to regulate appetite and body weight are leptin and ghrelin. Leptin is a hormone produced by adipose tissue (fat cells) that circulates to the brain and interacts with receptors in the hypothalamus to inhibit eating and control of body weight and fat distribution. In other words it tells the brain when one is full and should stop eating. Ghrelin is a hormone produced by stomach cells and gives the brain the order “hungry” and the person should eat. It has been found in most studies that leptin levels are increased in patients with OSA, also ghrelin levels were shown to be significantly higher, and that cause the individual to eat more. Because leptin levels are high in patients with OSA, it was postulated that OSA is associated with resistance to the weight reducing effects of leptin, which may in turn result increased appetite and weight gain. The appetite stimulating effects of ghrelin may well contribute to increased caloric intake and weight gain in patients with OSA. The table below summarises the association of OSA with the various hormones:
As shown, not only does obesity contribute to sleep disorders such as OSA, but sleep problems can also contribute to obesity. There are many factors associated with both OSA and obesity and while more research needs to be done regarding the relationship between them, it appears quite clear that the two are linked. The figure below shows the potential mechanisms formatting a vicious cycle where obesity may result in OSA and OSA may lead to weight gain:
Conclusions
3.1 Obstructive Sleep apnea (OSA) is a sleep disorder, more common among males aged 40-70.
3.2 OSA is characterised by loud snoring, nocturnal breathing pauses, choking and gasping.
3.3 If left untreated, OSA can cause excessive daytime sleepiness, fatigue, cognitive dysfunction, impaired work performance and decrements in health- related quality of life.
3.4 Overweight and obesity, body fat distribution, large neck girth and craniofacial and upper airway abnormalities are established risk factors for OSA.
3.5 It has been shown that obesity and OSA are associated with reduced physical activity.
3.6 The metabolic balance of sleep apnea and obesity seems to result from a complex balance between several regulatory hormones.
3.7 Not only that obesity contributes to sleep disorders such as OSA, but sleep problems can also contribute to obesity. It appears quiet clear that OSA and obesity are linked. “The chicken or the egg” questions existed and further research is needed.
3.8 Despite the FAA’s suspension of the new policy, the intentions that overweight pilots and ATCOs (BMI of 40 or greater) will be tested for OSA may be again relevant in the future.
Recommendations
4.1 To accept the paper as information.
References
ICAO Doc. 9966, Fatigue Risk Management Systems — Manual for Regulators. (2012).
Diabetes Care. (2008). Abdominal Fat and Sleep Apnea.
www.healthcentral.com. (2011). Can sleep deprivation cause obesity?
www.healthcentral.com. (2013). Obesity and Sleep Apnea: What’s the Connection?
National Sleep Foundation, www.sleepfoundation.org. (2013). Obesity and sleep.
American Medical Association. (2004). Risk Factors for Obstructive Sleep Apnea in Adults.
World Health Organization. www.who.int.
Air Transport News. www.atn.aero.


